This blog originally appeared in September on the Scottish Universities Insights Institute blog to accompany their Stigma in Childhood seminar series.
On 26th June I ran a workshop for the second Stigma in Childhood event, at the Scottish Universities Insight Institute at Strathclyde. This was an excellent opportunity to share some of my research on self-harm and young people, and hear from others about their views and experiences of the topic.
Self-harm (in the form of cutting, and overdosing mostly) is widely thought to be an increasing phenomenon among young people, though I would always urge caution when interpreting claims about ‘epidemics’ of self-harm. There is a similarly increasing amount of research addressing self-harm, the majority of which is carried out by clinical researchers working in psychiatry, or psychology. A smaller, but also growing, body of research uses qualitative, social scientific approaches to speak with young people themselves about self-harm. One of my research projects used a range of methods: an online, qualitative survey, interviews, and focus groups, in order to engage young people in Scotland, and further afield, in reflecting on self-harm.
A surprising theme that emerged in first few focus group discussions, and which I followed up in the qualitative survey, was that of ‘attention-seeking’.
Perhaps naively, I had expected that the (negative) phrase ‘attention-seeking’ might have fallen out of fashion, given that self-harm is so widely known and spoken about. Attention seeking had come up in my earlier research (interviews with adults who had self-injured, which I did in 2007-8) but since then information, awareness raising, and anti-stigma campaigns around self-harm have happened. Almost any information site, or leaflet on self-harm will emphasise that ‘it isn’t about attention-seeking’.
Blog on #endchildstigma workshop I ran in June @scotinsight https://t.co/h3V2tnvdrA pic.twitter.com/TTMpiyV6g5
— Amy Chandler (@DrAmyChandler) September 21, 2017
However, while I did find that young people who had self-harmed were critical of the idea of ‘attention-seeking self-harm’, my analysis also indicated that many still viewed any visible self-harm as potentially ‘attention-seeking’. Further, young people tended to emphasise the hidden nature of self-harm as a way of countering charges of ‘attention-seeking’. In a recently published paper, I discuss these findings further – suggesting that emphasising self-harm as a ‘hidden’ practice, may do more harm than good, by encouraging ideas that the ‘right way’ to self-harm is to hide it.
At the Stigma in Childhood workshop, I introduced some of the findings that are analysed in the paper, in order to prompt discussion among participants about the ways in which self-harm might be stigmatised.
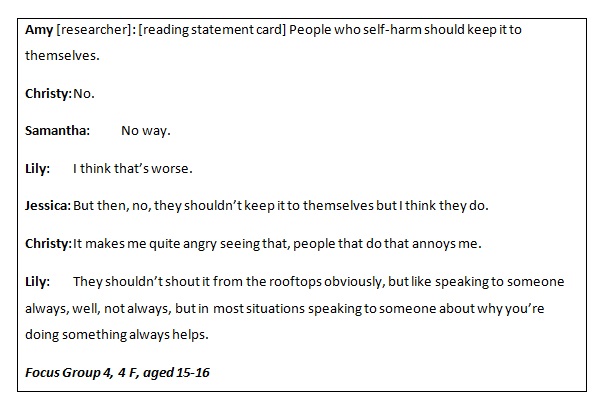
The discussion between Christy, Samantha, Lily and Jessica (all pseudonyms) generated a lot of interesting reflections in the workshops. I argued that Lily’s caution to people not to ‘shout it from the rooftops’ was well-meaning, but quite telling – inadvertently demonstrating that issues like self-harm shouldn’t be spoken of – at least not publicly. However, one workshop participant noted that ‘rooftops are dangerous places’, and suggested Lily was showing ‘care’ towards people who self-harm, helping to keep them safe. This useful point acknowledges that people who self-harm do continue to face stigmatising responses, and that this may shape their ability to talk openly about self-harm.
In my paper, I also reflect on the challenges faced by young people (and indeed anyone) who has self-harmed in a way that leaves visible (sometimes permanent) marks. One of the young people I interviewed, Jay, talked about her discomfort in some contexts with taking off layers of clothing if she was hot – because of an awareness that such an act could be interpreted by others as ‘attention-seeking’. Relatedly, Conrad, who took part in one of the focus group discussions, suggested that people who ‘showed’ their self-harm might be seeking help, rather than attention.
Questioning what ‘attention’ meant was a theme in both the research, and in the Stigma in Childhood workshop discussions. It is a word that can have negative connotations, especially when framed as ‘attention-seeking’ – the implication is that people who are attention-seeking do not deserve the attention they seek, or are going about seeking it in ‘the wrong way’. In both the research and workshop discussions, there was some willingness to challenge these negative views on attention-seeking; but there was also clear evidence that for many, self-harm remains associated in a negative way with the idea of ‘attention-seeking’, and that this contributes to the stigma experienced by those who self-harm.
You can find out more about the research with young people here, or take a look at a short animated film, based on the research findings, created by Yasmin (then aged 15), and animator Jim Stirk.
*Chandler, A. (2017, in press). “Seeking secrecy: a qualitative study of younger adolescents’ accounts of self-harm.” YOUNG: Nordic Journal of Youth Research.
Chandler, A. (2014). A sign that something is wrong? Young people talking about self-harm. CRFR Briefing No. 74. http://www.crfr.ac.uk/assets/SASHwebbriefing.pdf.
*Article is behind a paywall, but anyone wanting a copy who doesn’t have access should feel free to email me directly.